I’m finally discussing some current research on the diagnosis and treatment of a specific injury. In this week’s blog, I’m discussing the current Clinical Practice Guidelines for diagnosing and treating Patellofemoral Pain Syndrome (PFP). So if you have ever had knee pain related to squatting, running, descending stairs etc.. then this should be an informative read for you, providing you some direction in your ability to address your symptoms.
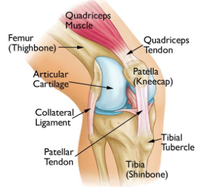
PFP is commonly referred to as “Jumper’s or Runner’s knee.” This condition involves, typically, insidious onset of pain behind or around the knee cap. This is a very common syndrome with an estimated prevalence of 25% up to 50% in the general population over their lifespan and does account for anywhere between 2-7.5% of people presenting for medical care. This syndrome most commonly affects youth athletes between the ages of 12-19 but some studies indicate a higher prevalence in the 50-59 year old age group.
Symptoms usually present with no specific injury and can come on slowly overtime. Typically there is worsening of pain with lower-limb loading (eg, squatting, prolonged sitting, ascending/descending stairs, jumping, or running, especially with hills). There is poor correlation between internal derangement of tissue or cartilage damage and symptoms, and therefore a clinical diagnosis based on a cluster of symptoms associated with pain reports during squatting, descending stairs, and knee flexion positions like prolonged sitting should be used. Your medical provider and rehab specialist should be looking at these things as the best supported way to diagnosis this condition.
Once there is a clear idea that you are dealing with PFP, a tailored strengthening program and symptom management program should be developed based on these well supported treatment approaches. This really should be a staple in all treatment approaches.
Have you ever been told you have flat feet?? Well, it turns out that, flat feet in combination with an increased knee valgus (inward tilt) angle may contribute to symptoms early on.

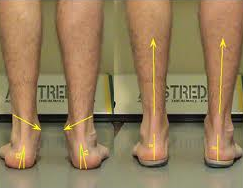
Therefore, within the first 6 weeks, a pronation controlling foot orthotic may provide relief from symptoms temporarily. Studies also show that over-the-counter orthotics provide just as much support for this condition as do custom orthotics. Talk to your therapist about one that might work for you.
In addition within the first 6 weeks, patellar taping can provide relief for symptoms and can be a very cost effective way to address symptoms early on.

With that that being said, the major focus for individuals with PFP should be gluteal and quadriceps specific strengthening exercises. These should be in both the open chain (resisted knee extension, hip raises, banded stepping etc..) as well as in the closed chain (weighted cross over step ups, progressive resisted squats and lunges etc..). This program should be set over a 6-8 week time frame allowing for true strength gains.
So, If you are someone that is battling anterior knee pain associated with tasks such as running, squatting, descending stairs, or sitting for prolonged periods and are looking for a resolution to your problem, talk to a physical therapist or musculoskeletal healthcare expert today to follow these research supported guidelines to aid in your recovery.
Hope you enjoyed and thanks for reading!
Dr. Luke
Citation: Willy, Richard Et. al. Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy, 2019 Volume:49 Issue:9 Pages:CPG1–CPG95 DOI: 10.2519/jospt.2019.0302